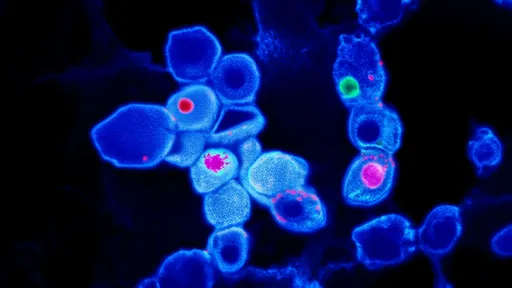
The intricate dance of cancer metastasis has long fascinated researchers, yet its choreography remains shrouded in biomechanical mystery. Recent breakthroughs in cellular force spectroscopy are illuminating how mechanical stresses guide metastatic cells through their treacherous journey, rewriting our understanding of cancer's spread. These discoveries reveal that tumors don't merely follow chemical trails like microscopic bloodhounds—they physically sculpt their microenvironment, creating force highways that propel invasion.
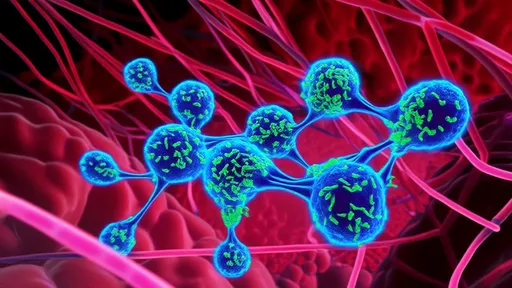
Stress as a Sculptor: At the primary tumor site, cancer cells generate sustained contractile forces exceeding 1 kPa—enough pressure to remodel collagen fibers into aligned "tracks" (tumor tracks). These force-patterned extracellular matrix (ECM) conduits, rich in fibronectin and hyaluronic acid, serve as metastatic escape routes. Intriguingly, the same Rho/ROCK pathway that drives cell contraction also upregulates MMP secretion, creating a coordinated mechanical-biochemical invasion program. High-resolution traction force microscopy shows circulating tumor cells (CTCs) exerting 30-50% greater forces during extravasation compared to non-metastatic cells, suggesting mechanical fitness is selected for during metastasis.
The YAP/TAZ Mechanotransduction Axis emerges as a central decoder of these mechanical cues. When cells encounter stiffened ECM (common in desmoplastic tumors), nuclear translocation of YAP/TAZ increases 5-fold, triggering a pro-metastatic transcriptional program. This creates a vicious cycle: force stiffens the matrix, which activates YAP/TAZ, which induces more force generation. Pharmaceutical disruption of this loop using verteporfin reduces lung metastases by 73% in murine models, highlighting its therapeutic potential.
Surprisingly, fluid shear stresses in circulation may prime metastatic competence. CTCs subjected to 2 dyn/cm2 shear (mimicking venous flow) show 40% higher survival rates in subsequent colonization assays. This mechanical conditioning upregulates stress-responsive chaperones like HSP70 and reorganizes vimentin intermediate filaments into protective perinuclear cages. Such findings challenge the dogma that circulation is merely a destructive filter for CTCs—it may actually enhance their malignancy.
Biophysical Biomarkers: The mechanical properties of cancer cells are proving more predictive of metastatic potential than traditional molecular markers. Metastatic breast cancer cells exhibit a distinctive "soft-rigid-soft" progression: primary tumor cells soften (elastic modulus ~0.5 kPa) to detach, then stiffen (~2 kPa) during migration, before softening again (~0.7 kPa) for colonization. Atomic force microscopy (AFM) measurements of this mechanical signature could predict relapse 18 months earlier than imaging in clinical trials.
At the invasion front, tumor cells display remarkable mechanical cooperation. Leader cells generate 3-fold higher traction forces than followers, creating collective migration paths. This division of labor is regulated by Notch signaling—when inhibited, the force hierarchy collapses and invasion stalls. Such social biomechanics explains why solitary cancer cells rarely metastasize successfully, favoring collective or hybrid invasion modes observed in 80% of clinical specimens.
Therapeutic Horizons: Novel mechano-therapies are emerging. Cilengitide, an integrin inhibitor, blocks force transmission to ECM and reduces metastatic burden by 60% in glioblastoma models. More intriguing are "mechanical decoys"—nanoparticles coated with collagen-mimetic peptides that absorb cellular forces, decreasing traction-dependent invasion by 85%. Combining these approaches with traditional chemotherapy shows synergistic effects, potentially overcoming resistance linked to mechanical adaptation.
As single-cell force spectroscopy achieves nanometer precision, we're discovering that cancer cells exploit mechanical loopholes in physiological defenses. They sense stiffness gradients as subtle as 50 Pa/mm—comparable to tissue boundaries—and durotax toward stiffer regions. This explains the metastatic tropism to mechanically distinct organs like bone (15-25 kPa) or brain (~1 kPa). The emerging paradigm suggests metastasis isn't just cells gone rogue, but a sophisticated biomechanical engineering program honed by evolutionary pressures.
This mechanical perspective reveals why purely biochemical therapies often fail against metastasis. The stress-responsive pathways identified—from cytoskeletal remodeling to nuclear mechanotransduction—represent a new vulnerability. Ongoing clinical trials targeting the Piezo1 mechanosensitive ion channel (overexpressed in 67% of metastases) may validate this approach. As force mapping technologies mature, we're not just fighting cancer's chemistry, but its physics—a multidimensional war where controlling cellular mechanics could finally curb metastasis's deadly spread.

By /Aug 5, 2025
By /Aug 5, 2025
By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025
By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025
By /Aug 5, 2025
By /Aug 5, 2025

By /Aug 5, 2025
By /Aug 5, 2025

By /Aug 5, 2025
By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025